Opioid Use Disorder (OUD) is a medical condition characterized by a problematic pattern of opioid use that leads to significant impairment or distress. Opioids are a class of drugs that include prescription pain relievers like oxycodone, hydrocodone, morphine, and illegal drugs like heroin.
Individuals with OUD often exhibit symptoms such as:
- Strong cravings for opioids.
- Difficulty controlling opioid use.
- Continued use of opioids despite negative consequences, such as health problems or relationship issues.
- Tolerance, meaning they need higher doses of opioids to achieve the desired effects.
- Withdrawal symptoms when not using opioids.
Opioid Use Disorder can have severe consequences, including overdose and death. Treatment typically involves a combination of medication (such as methadone, buprenorphine, or naltrexone) and behavioral therapies to help individuals manage cravings, avoid relapse, and address underlying issues contributing to their substance use.
Opioid Use Disorder Resources
Websites
FindTreatment.gov
The confidential and anonymous resource for persons seeking treatment for mental and substance use disorders in the United States and its territories. Available in Spanish.
Get the Facts on Opioid Use Disorder
Opioids are a class of drugs that include prescription pain relievers, synthetic opioids and heroin. These natural or synthetic chemicals interact with opioid receptors on the nerve cells in the body and brain and reduce feelings of pain.
Johns Hopkins Medicine
This website contains Opioid Use Disorder information provided by Johns Hopkins Medicine.
American Psychiatric Association
This website includes opioid use disorder information and resources for patients and families from the American Psychiatric Association (APA).
988 Suicide & Crisis Lifeline – Call. Text. Chat.
The 988 Lifeline provides 24/7, free and confidential support for people in distress, prevention and crisis resources for you or your loved ones, and best practices for professionals in the United States.
Tools & Resources
What The Cut: Reno’s Drug Checking Program
What The Cut is a free, confidential drug checking project in Reno, Nevada that analyzes small samples to show people what is actually in the local drug supply. The site shares community testing results, trends, and safety information to help people stay informed and reduce risks.
Opioid Treatment Program Directory
Find treatment programs in your state that treat addiction and dependence on opioids.
Providers Clinical Support System-Medications for Opioid Use Disorder (PCSS-MOUD)
Trains health professionals to provide effective, evidence-based, medication treatments to patients with opioid use disorder in primary care, psychiatric care, substance use disorder treatment, and pain management settings.
Start Your Recovery Nevada Treatment Locator
Start Your Recovery recently developed a comprehensive directory of support resources in Nevada where individuals can: Find local treatment options vetted by the Substance Abuse and Mental Health Services Administration; Filter to find free and low-cost support options; and Find support groups and other important non-clinical resources.
Medications for Addiction Treatment (MAT) Resource Library
The MAT Resource Library is supported by the Los Angeles County Health Agency and Department of Public Health, Substance Abuse Prevention and Control. The site provides practical information on Medications for Addiction Treatment (MAT) for providers across health systems (e.g., physical health, mental health, and substance use disorder systems), as well as for patients.
Nevada Fentanyl Test Strip Finder
A list and map of Fentanyl Test Strip Distribution Sites in Nevada.
Nevada Overdose Reversal Medication Finder
Find naloxone and overdose reversal medications in Nevada.
The Opioid Guide: A Resource Guide for Practicing Psychologists
A guide from the American Psychological Society with information for practicing psychologists on opioids, their use, and effective treatments.
Screening Tools
Adopt SBIRT offers training and technical assistance on the use of screening assessments.
Never Use Alone
Toll-free national overdose prevention, detection, life-saving crisis response and medical intervention services for people who use drugs while alone. Never Use Alone’s peer operators are available 24-hours a day, 7 days a week, 365 days a year.
Las Vegas Harm Reduction Center
Trac-B seeks to improve the quality of life of those affected by substance use disorders including our clients, their loved ones, and their communities. Trac-B Exchange provides harm reduction services and supplies to people engaged in the sex trade and people who are injecting or misusing drugs or other substances and are at risk for violence and communicable diseases including Hepatitis C and HIV.
Medication for Opioid Use Disorder (MOUD) Toolkit for Peer Recovery Specialists
This toolkit is a resource for Peer Recovery Specialists (PRSs) to feel equipped to discuss MOUD with providers, people seeking recovery, and others with questions about this treatment option.
Posters & Infographics

Opioid Trifold Brochures
Opioid Information Brochures for Providers or Consumers help educate on opioids and opioid use, including effects of opioid use, pregnancy and opioid use, medications for opioid use including opioid overdose reversal medications, and treatment options for persons using opioids.
Download or request free hard copies

Prevent Addiction Fact Sheet
This face sheet contains information for patients about preventing opioid addiction.
Download the Fact Sheet
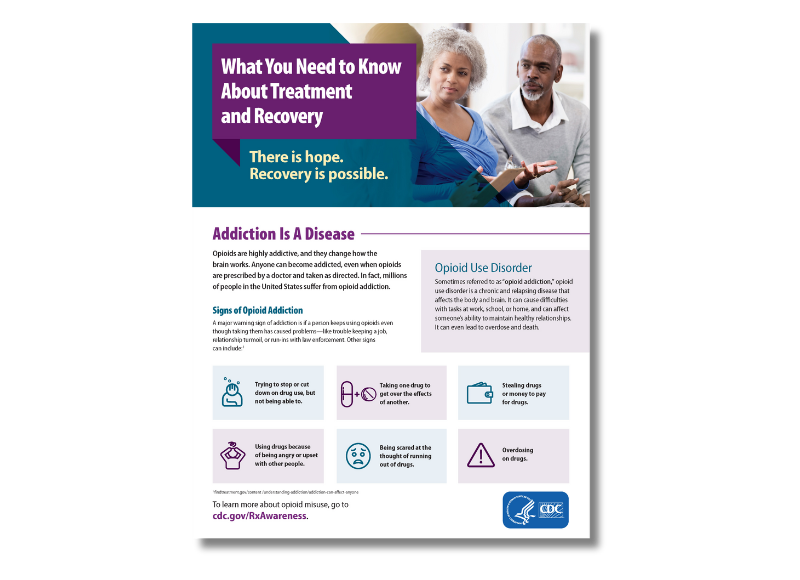
Opioid Use Disorder Treatment and Recovery Fact Sheet
This fact sheet contains important information about treatment and recovery of opioid use disorder for patients, families and friends.
Download the fact sheet
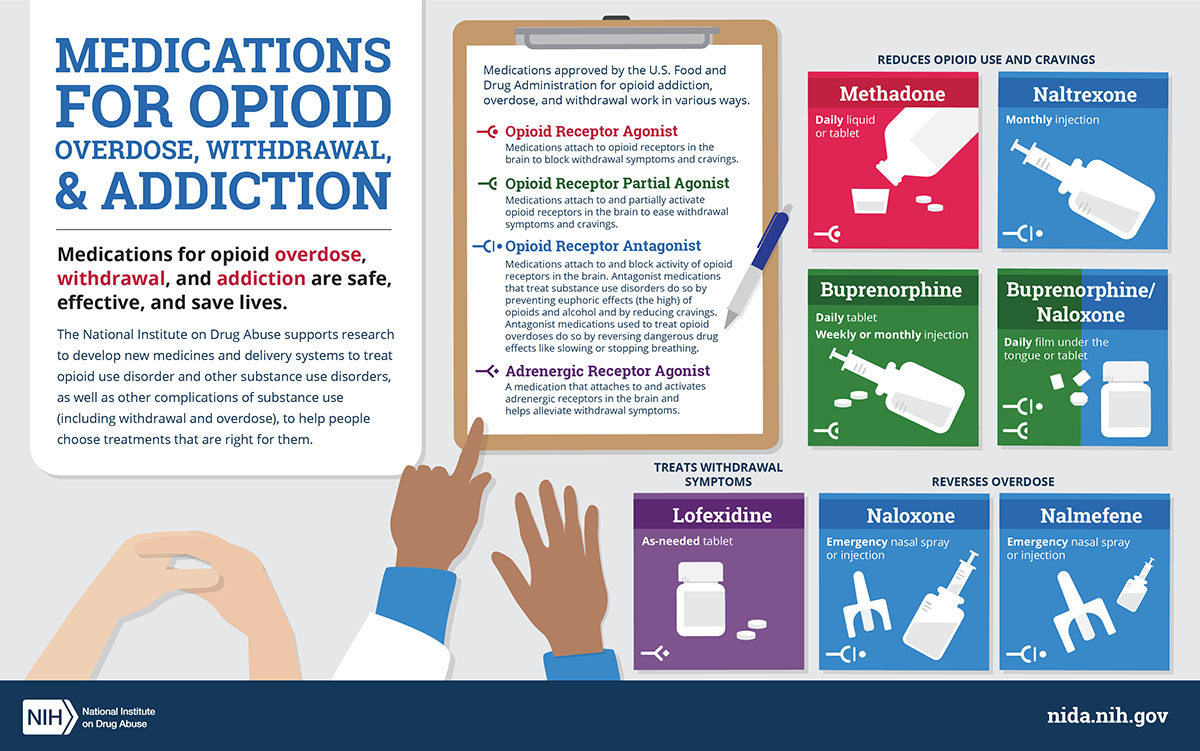
Medications for Opioid Use Disorder (MOUD) Infographic
This infographic shows different types of medications approved by the U.S. Food and Drug Administration for opioid overdose, withdrawal, and addiction.
Download the infographic
Publications
Brief: Tobacco and Opioids
The brief explores the connection between tobacco use and opioid addiction, highlighting how smoking may increase the risk of opioid misuse and how addressing tobacco dependence can improve substance use recovery outcomes. It emphasizes the need for integrated treatment approaches in substance use disorder programs, including tobacco cessation interventions, to enhance recovery success. The document also outlines policy and healthcare strategies to support dual cessation efforts, such as insurance coverage, clinical screening, staff training, and tobacco-free campus policies.
When Your Child, Teenager, or Adult Son or Daughter has a Mental Illness or Substance Use Disorder, Including Opioid Addiction: What Parents Need to Know about HIPAA
This resource explains how HIPAA allows healthcare professionals to share health information with a patient’s loved ones during emergencies or dangerous situations, such as an opioid overdose, when doing so is in the patient’s best interest. It clarifies that health providers can disclose information to family and caregivers without patient consent if the patient is incapacitated or poses a serious and imminent threat to their health. Additionally, it outlines limitations on sharing information for patients who have decision-making capacity and recognizes state laws regarding personal representatives who have authority over a patient’s health information.
How HIPAA Allows Doctors to Respond to the Opioid Crisis
This resource explains how HIPAA allows healthcare professionals to share health information with a patient’s loved ones during emergencies or dangerous situations, such as an opioid overdose, when doing so is in the patient’s best interest. It clarifies that health providers can disclose information to family and caregivers without patient consent if the patient is incapacitated or poses a serious and imminent threat to their health. Additionally, it outlines limitations on sharing information for patients who have decision-making capacity and recognizes state laws regarding personal representatives who have authority over a patient’s health information.
How HIPAA Helps Family and Friends Stay Connected with Loved Ones Who Have a Substance Use Disorder, including Opioid Abuse, or a Mental or Behavioral Health Condition
This resource explains how HIPAA allows healthcare providers to share necessary health information with family and friends of individuals with substance use disorders (including opioid abuse) or mental health conditions when it is in the patient's best interest. It outlines how providers can notify loved ones in emergencies, share relevant treatment details for caregiving purposes, and grant full access to personal representatives who have legal decision-making authority.
Wound Care & Medical Triage for People Who Use Drugs and the Programs That Serve Them
This comprehensive guide provides information and recommendations regarding general health, safer use practices, common viral, fungal, parasitic, and other injection-related infections, overdose and overamp, tapering, withdrawal, medications for opioid use disorder, and seeking medical care.
Opioid Use and Opioid Use Disorder in Pregnancy: A Joint Opinion of the ACOG’s Committee on Obstetric Practice and ASAM
The Society of Maternal–Fetal Medicine endorses this document. This Committee Opinion was developed by the American College of Obstetricians and Gynecologists’ Committee on Obstetric Practice in collaboration with committee members Maria A. Mascola, MD, MPH; Ann E. Borders, MD, MSc, MPH; and the American Society of Addiction Medicine member Mishka Terplan, MD, MPH.
Opioid Use Disorder
This activity focuses on the critical evaluation and management of opioid use disorder (OUD), a pervasive condition significantly diminishing patients' quality of life and contributing to a widespread epidemic in the United States.
Heroin, Fentanyl, & Other Opioids: A Comprehensive Resource for Families with a Teen or Young Adult Struggling with Opioid Use
Fueled by drugs like heroin, fentanyl and the misuse of prescription pain pills, the opioid epidemic in our country has impacted countless families. To help address this, the Partnership for Drug-Free Kids created a new eBook — Heroin, Fentanyl & Other Opioids: A Comprehensive Resource for Families with a Teen or Young Adult Struggling with Opioid Use. Parents and families need to be prepared with the knowledge and skills to identify opioids, spot early use and take action effectively.
Webinars & Online Learning
Current News & Research
What The Cut: Reno’s Drug Checking Program
What The Cut is a free, confidential drug checking project in Reno, Nevada that analyzes small samples to show people what is actually in the local drug supply. The site shares community testing results, trends, and safety information to help people stay informed and reduce risks.
Benzimidazole-Opioids (Nitazenes)
The DEA's report on benzimidazole-opioids (Nitazenes) highlights the rising abuse of synthetic opioids from this structural class, which have been linked to numerous toxicology cases and deaths since 2019. These substances, which act as mu-opioid receptor agonists, pose significant public health risks due to their potency and lack of medical use in the United States. Their presence in the illicit drug market underscores the ongoing opioid epidemic and the dangers of emerging synthetic drugs.
Project AMPED
This is a multi-year, mixed methods study in Nevada and New Mexico is examining the patterns, reasons for, and health concerns related to methamphetamine use and opioid use.
Opioid Use Disorder Assessment Tools and Drug Screening
Opioid use disorder risk assessment tools cannot be used in isolation. In combination with standardized clinical examination, and, when indicated, urine drug screening, a validated risk assessment tool, improves the ability to detect opioid misuse. Even though no single tool has been shown to have both high interobserver reliability and high sensitivity, the standardized approach has still been shown to be superior to subjective care giver assessment. This article will provide a global approach to risk assessment in addition to reviewing the available tools.
