Co-published by CASAT OnDemand and the Nevada Opioid Center of Excellence (NOCE)
As temperatures across the West continue to rise, extreme heat has become more than a seasonal inconvenience—it’s a growing public health crisis. In Nevada, people without access to stable housing or cooling resources face serious health risks during heat waves. Substance use, certain medications, and chronic health conditions can also increase vulnerability. Understanding who’s most at risk—and how to stay safe—is critical as our summers grow longer and hotter.
According to the Southern Nevada Health District (2024), 475 heat-associated deaths were reported in Clark County in 2024, marking a 60% increase over the previous year. Of those deaths, over half involved substance use, particularly methamphetamine (60%) and alcohol (9%), and 35% involved people experiencing homelessness. These figures underscore the urgent need for coordinated outreach, education, and life-saving resources.
What Is Heat Illness?
Heat illness refers to a range of medical conditions caused by the body’s inability to stay cool. These can escalate quickly from mild to life-threatening:

Heat rash: Skin irritation caused by excessive sweating, often on the neck, upper chest, or elbow creases.

Heat cramps: Painful muscle spasms, usually in the legs, arms, or abdomen, due to dehydration and electrolyte loss.

Heat fainting: Dizziness or fainting from prolonged standing or sudden posture changes.

Heat exhaustion: Symptoms include heavy sweating, weakness, confusion, nausea, headache, and cool, moist skin.

Heat stroke: A medical emergency marked by a core temperature of 103°F or higher, hot/red skin, confusion, vomiting, or unconsciousness.
Risk factors for heat-related illness include dehydration, certain medical conditions, alcohol and caffeine consumption, blood pressure, lack of acclimation, missed meals, physical condition, age, and weight.
School of Public Health, University of Nevada, Reno, 2025
Understanding the Risks: Why People Who Use Drugs Are Especially Vulnerable
Extreme heat poses health risks for everyone, but people who use drugs (PWUD) and those without access to stable housing face additional challenges, including:
Limited access to air-conditioning, showers, or other vital ways to stay.
Increased exposure to heat when using drugs in uncooled spaces such as parked cars, unsheltered areas, or housing without air-conditioning.
Higher risk of heat-related illness due to how certain substances affect the body’s ability to regulate temperature.
Different drugs affect the body in different ways, making some substances especially risky to use in hot weather. The following chart from the New York State Department of Health (2024) illustrates how various substances increase the risk of heat-related illness.
| Substance | Heat-Related Risks |
| Alcohol | Heatstroke: When combined with higher temperatures, alcohol may cause the body to lose its ability to regulate its own temperature effectively. Dehydration: Alcohol is a diuretic, which promotes water loss through urine at a quicker rate than other liquids. |
| Opioids | Sweating: Opioids can cause excessive sweating – hyperhidrosis. Dehydration: Opioid withdrawal can cause sweating, runny nose, watery eyes, nausea, vomiting and diarrhea, which lead to dehydration. Those who regularly take opioids have found that their efficacy is reduced in warmer weather. They may potentially take higher doses on warmer days. |
| Stimulants | Dehydration: Stimulants – cocaine, crack cocaine, methamphetamine, prescription amphetamines – increase core body temperature and the risk of overheating and dehydration. Heatstroke: Stimulants impair the ability of the cardiovascular system to cool the body and decrease the sense of discomfort associated with heat that would lead to heat-avoidant behaviors. Sunburn: Prescription stimulants – Adderall,™ Ritalin™ – may cause a person to become sunburnt more easily. Using drugs to the point of intoxication could cause an increased risk of sunburn if a person is outside/sleeping/nodding out more than anticipated and without sunscreen. |
| MDMA (3,4-Methylenedioxy- methamphetamine)/Ecstasy) | Heatstroke: MDMA (3,4-Methylenedioxymethamphetamine) can decrease the sense of discomfort associated with heat that would lead to heat-avoidant behaviors. Dehydration: MDMA (3,4-Methylenedioxymethamphetamine) – also known as Ecstasy or Molly – increases core body temperature and can overheat the body even when used in normal temperatures. |
| Antidepressant or Antipsychotic Medications | Heatstroke: Prescription medications, such as antidepressant and antipsychotic medications, can negatively impact the body’s ability to regulate temperature and increase the risk of heatstroke. |
Stimulants, Heat, and the Risk of Overamping
Extreme heat increases the risk of overamping—a potentially life-threatening reaction to stimulant use. Overamping happens when the body becomes overwhelmed by the effects of substances like cocaine, methamphetamine, or prescription amphetamines. Symptoms may include anxiety, paranoia, rapid heartbeat, overheating, or even loss of consciousness.
When temperatures reach 75°F or higher, these risks become more pronounced. People may experience more intense effects or overdose with smaller amounts of stimulants than usual (New York State Department of Health, 2024). Heat also places extra strain on the cardiovascular system, making it harder for the body to cool itself. At the same time, stimulants reduce a person’s ability to recognize discomfort, meaning early signs of heat illness—like dizziness or confusion—can go unnoticed until it’s too late.
Tips to Stay Safe in Extreme Heat
Hot weather can make drug use more dangerous by increasing the risk of dehydration, overheating, and overdose. Here are some tips to help people who use drugs stay safer during extreme heat:

Stay Hydrated
Drink plenty of water, even if you don’t feel thirsty. Sports drinks can help replace salts and minerals lost through sweating. Dehydration can cause cracked/dry lips. Use lip balm and drink water.

Keep Cool
If you’re feeling too hot, wear a wet scarf, bandana, or shirt to cool down. Use sunscreen and a ventilated hat—like straw or mesh—even on cloudy days. Avoid hot, heavy meals since they raise your body temperature. Use local cooling centers, pools, or splash pads, and try to stay in shaded or air-conditioned places like libraries or service organizations whenever possible.

Plan Ahead
Hot weather can intensify drug effects and increase the risk of overdose. Try to reduce your dose and frequency, and use in safe, familiar places with people you trust. Avoid using in parked cars, even briefly, as temperatures inside can rise quickly and become deadly.

Stay Connected and Never Use Alone
Stay in touch with trusted friends, support groups, or harm reduction organizations that can provide aid and support during extreme heat. Remember that extreme heat can intensify the effects of some drugs and increase the risk of overdose. If you’re with others, stagger use so someone is alert and able to respond in an emergency.
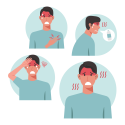
Watch for Signs of Heat Illness
Watch for symptoms of heat-related illness, such as: These can signal dehydration, heat exhaustion, or heatstroke.
- Dizziness
- Nausea
- rapid heartbeat
- confusion
- clammy skin
- not sweating despite feeling hot
If you notice any of these signs, move to a cooler area, rest, and drink water. Seek medical attention if symptoms are severe.

Know What to Do in an Emergency
If someone is experiencing severe symptoms—such as vomiting, disorientation, staggering, irrational behavior, loss of consciousness, or convulsions—call 911 immediately. Be ready to give emergency responders the most accurate location possible (School of Public Health, University of Nevada, Reno, 2025).
How Communities and Organizations Can Help
Community organizations play a key role in protecting our most vulnerable populations during periods of extreme heat. Here are a few steps organizations can take to reduce risk and support their clients:
- Distribute supplies like cooling towels or bandanas, ice packs, water bottles, and information about local cooling centers and swimming pools.
- Before extreme heat events, provide extra doses of naloxone and drug testing strips.
- Educate participants about how different substances affect the body in the heat, and share practical tips for staying safe (New York State Department of Health, 2024).
As Nevada continues to face rising temperatures and more frequent heat waves, it is essential to recognize the heightened risks for people who use drugs and those without stable housing. These intersecting challenges demand urgent, coordinated action. Public health professionals, outreach teams, and community members all have a role to play—whether that’s checking on neighbors, sharing heat safety information, or distributing cooling and overdose prevention supplies. By planning ahead and acting together, we can help save lives and build more resilient communities.
References
New York State Department of Health. (2024). Extreme heat and people who use drugs: Information for harm reduction organizations. U.S. Department of Health. https://www.health.ny.gov/diseases/aids/consumers/prevention/oduh/docs/extreme_heat_hro.pdf
School of Public Health, University of Nevada, Reno. (2025). Volunteer training: Heat illness awareness & response at Hot August Nights [PowerPoint slides].
Southern Nevada Health District. (2024). Heat-associated deaths & emergency department visits – 2024 report. https://media.southernnevadahealthdistrict.org/download/heat-death-report-october-2024.pdf





